Challenge: 250+ provider plan files/month from multiple partners needed normalization, validation, and publishing to downstream systems. Manual processing caused backlogs and data inaccuracies.
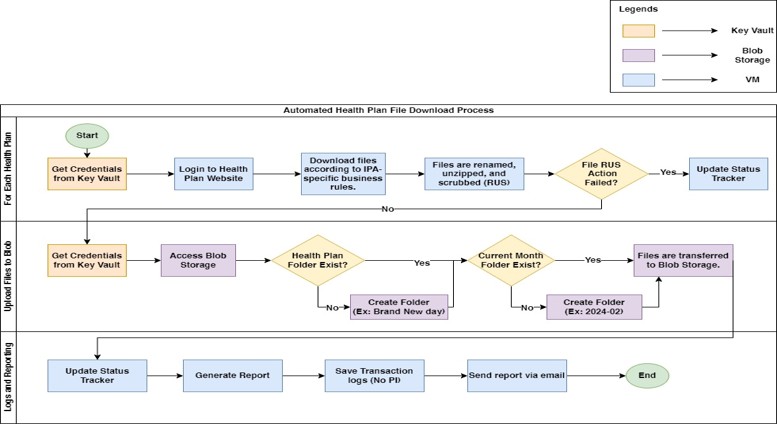
Solution: Automated ingestion pipeline (watch → extract → standardize → validate → publish) with business rules and quality checks.
Impact: ~70% reduction in manual work, faster plan publish cycles, improved accuracy, scalable for monthly/quarterly releases.
RPA + Rules Engine
OCR & Validation
Secure Connectors